Digital transformation in healthcare refers to the comprehensive integration of digital technologies into all aspects of the healthcare industry, fundamentally changing how healthcare services are delivered, managed, and improved and creating the need for healthcare product management. This transformation involves the adoption of a wide array of digital tools and innovations that streamline operations, fight burnout, and enhance patient care.
Whether operational in nature, like Electronic Data Interchange (EDI) for one-off, bill-only implants, or as close to patients as a smart bed that detects pressure ulcers, digital innovation in healthcare has the potential to radically transform the system and disrupt the status quo to effect positive change.
The article below highlights 8 healthcare digital transformation trends accompanied by real-world examples and their results.
If you’re interested not only in the what but also the how of digital transformation, check out Product School’s latest white paper on digital transformation in healthcare, highlighting opportunities for Healthcare Leaders to develop and execute digital strategies that stick.
Healthcare Industry Report
Dive into the latest research about digital transformation in healthcare in this white paper from Product School. Spark ideas with 6 case studies and over 25 digital solutions from operations to pharmaceuticals to primary care and more.
Download report
1. Telemedicine and Remote Patient Monitoring
In the same way that the global pandemic changed the way we approach remote work, even when patients could return to seeing their doctors in person, they prefer a virtual visit in many instances and have come to expect easy, frictionless scheduling and delivery.
Growth and adoption of telemedicine among patients
The telehealth market is experiencing unprecedented growth, with a projected compound annual growth rate (CAGR) that could see the market reaching up to $912 billion by 2033. This surge is driven by the increasing acceptance and utilization of telehealth services among both providers and patients.
The best part of this trend is that it’s least partly patient-driven. 94% of patients who have tried telehealth services would use them again, especially for the following services:
Prescription Refills: 80% of patients prefer using telehealth for prescription refills.
Medication Recommendations: 72% of patients favor telehealth consultations for discussing medication options.
Test Results: 71% of patients prefer receiving test results through telehealth platforms.
Mental health visits: Just over half of patients (57%) prefer virtual counseling and other mental health services.
Examples of positive results from the virtual healthcare trend
Virtual care on a Google Cloud-based platform
A telehealth platform that offers virtual preventative care services for menopausal patients reduced insurance charges for acute care by 50%.
Digital triage through images
A dedicated digital channel for dermatological triage allows patients to send images of their skin conditions to specialists for prompt evaluation. This system improves resource allocation and speeds up response times, with 75% of cases managed within the initial consultation. Moreover, nearly all patients with serious conditions receive surgery within two weeks.
Benefits of the telehealth trend
Increased accessibility: Telemedicine breaks down geographical barriers, making healthcare accessible to patients in remote or underserved areas. This is particularly beneficial for individuals with mobility issues or those requiring frequent follow-ups.
Convenience and efficiency: Patients can receive medical consultations and monitoring from the comfort of their homes, reducing the need for travel, rescheduling, and waiting times.
Cost savings: By reducing the need for in-person visits, telemedicine and remote patient monitoring can lower healthcare costs for both providers and patients. Additionally, early detection and continuous monitoring can prevent complications, further driving down costs.
Better resource management: Healthcare providers can optimize their resources by managing more patients remotely, even working from home themselves, helping reduce burnout.
2. Improved Interoperability: Electronic Data Interchange (EDI) and Electronic Health Record (EHR)
Interoperability in healthcare refers to the seamless exchange and use of information across different healthcare systems and organizations. It is a cornerstone of digital transformation in healthcare. Two key examples of interoperability in healthcare are Electronic Health Records (EHR) interoperability and Electronic Data Interchange (EDI).
EHR interoperability makes comprehensive and continuous care possible, as it ensures that all healthcare providers involved in a patient's treatment have access to the same, up-to-date information. EDI automates the exchange of business documents and data between healthcare systems in a standardized format. This automation streamlines administrative and operational processes, reducing manual intervention and errors.
Interoperability Innovations and Trends
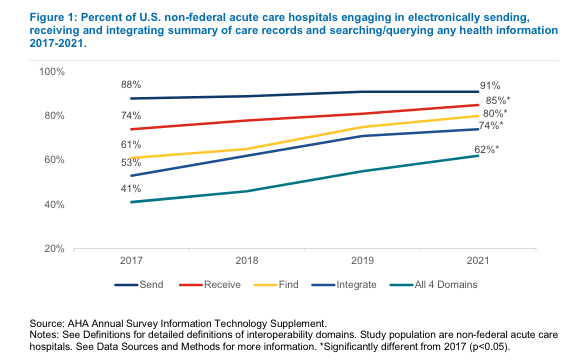
The percentage of US hospitals that engaged in all aspects of exchange (send, receive, query) and integrating of summary of care records into EHRs increased by 51% from 2017-2021 as shown by the Office of the National Coordinator for Healthcare Information Technology:
An example of EDI implementation is the healthcare organization that converted its manual purchasing processes to EDI for one-off, bill-only implants. This automation included tasks such as serial number alignment, resulting in a 75% decrease in the purchase order to invoice time—from an average of 10-14 days to just 2-4 days.
Benefits of EDI and EHR
Enhanced Care Coordination: Ensures that all members of a patient’s care team can access the same medical history, treatment plans, and medication lists, reducing the risk of errors and duplicate tests.
Improved Patient Outcomes: Allows for better-informed clinical decisions by providing healthcare providers with complete and accurate patient information.
Operational Efficiency: Automates routine administrative tasks such as billing, supply orders, and insurance claims, speeding up transactions and reducing the risk of errors. Reduces the administrative burden associated with manual data entry and patient paperwork.
Cost Reduction: Reduces the costs associated with manual data entry and paperwork, leading to significant cost savings for healthcare organizations.
Improved Accuracy: Minimizes the likelihood of errors in business transactions, ensuring more accurate and reliable information handling.
3. Artificial Intelligence and Machine Learning
Artificial Intelligence (AI) and Machine Learning (ML) are at the forefront of healthcare digital transformation trends, driving significant advancements in diagnostics, treatment planning, and operational efficiency. AI and ML technologies process vast amounts of data to identify patterns, predict outcomes, and suggest interventions. This capability is transforming various aspects of healthcare, from clinical decision support to administrative functions.
Examples of AI in Healthcare
Prediction-Informed Dashboards
AI-powered prediction-informed dashboards were integrated with Electronic Health Record (EHR) systems to support daily bed-placement decisions in hospital wards with over 80% accuracy, helping healthcare providers optimize bed allocation, reduce patient wait times, and improve overall hospital efficiency.
AI-Powered Surgery Scheduler:
A self-learning, real-time AI-powered surgery scheduler enhanced the accuracy of surgical planning by 35%, reduced overtime hours by 21%, and increased the overall occupancy rate by 12%. The scheduler continues to refine its predictions based on new inputs to optimize surgical resources and personnel.
Benefits of AI-powered solutions in healthcare
Enhanced diagnostic accuracy: AI algorithms can analyze medical images, lab results, and patient records with high precision, assisting clinicians in diagnosing diseases more accurately and at earlier stages.
Operational efficiency: AI-driven automation of administrative tasks, such as scheduling, billing, and inventory management reduces the administrative burden on healthcare staff and cuts operational costs.
Predictive analytics: AI can analyze historical and real-time data to predict patient outcomes, identify at-risk patients, and suggest preventive measures. For example, predictive analytics can forecast hospital admission rates, helping healthcare facilities manage resources more effectively.
Furthermore, machine learning models can predict how individual patients will respond to different treatments based on their genetic makeup, lifestyle, and medical history.
Streamlined Workflows: By integrating AI into EHR systems and other healthcare platforms, providers can streamline workflows, reduce redundancies, and increase interoperability for more coordinated and efficient patient care.
4. Strategies for Enhancing Cybersecurity in Healthcare
As healthcare systems increasingly adopt digital technologies, the importance of robust cybersecurity measures has become more critical than ever to protect sensitive patient data, ensure the integrity of healthcare operations, and maintain patient trust.
Current Challenges in Healthcare Cybersecurity
Research indicates a gap in the enforcement and adoption of robust security measures:
Lax security protocols
1 in 5 healthcare workers report that security protocols are not strictly enforced in their organization.
Inconsistent use of multi-factor authentication
Just 39% report using multi-factor authentication consistently.
Ineffective Security Training
Only half feel that security training is efficient and keeps up with new technologies like AI, and 19% agree that the training they do get is not relevant to their jobs.
Cybersecurity trends in healthcare
To address these challenges, healthcare organizations are looking at how to implement robust cybersecurity measures as part of their healthcare digital strategy in the following ways:
Strengthening security protocols: Healthcare organizations must enforce strict security protocols, including the use of multi-factor authentication, to protect against unauthorized access.
Regular security training: Continuous and up-to-date security training for all healthcare staff is crucial. Training programs should cover the latest cybersecurity threats and best practices for preventing breaches.
Implementing advanced security technologies: Utilizing advanced cybersecurity technologies, such as AI and machine learning, can help detect and respond to threats in real time. AI can analyze network traffic patterns to identify unusual activities and prevent potential breaches, as seen in the banking sector.
Encrypting Data: Encrypting sensitive data ensures that even if it is intercepted, it cannot be read without the appropriate decryption key. This adds an extra layer of protection for patient information.
Conducting Regular Security Audits: Regular security audits and risk assessments can help identify vulnerabilities in healthcare information systems. These audits enable organizations to address weaknesses before they can be exploited by cybercriminals.
Developing Incident Response Plans: Having a well-defined incident response plan ensures that healthcare organizations can quickly and effectively respond to cybersecurity incidents, minimizing damage and restoring operations as swiftly as possible.
5. Software as Medical Device (SaMD) and Internet of Medical Things (IoMT)
The convergence of software and connected medical devices provides innovative solutions that can enhance patient care, streamline clinical workflows, and improve health outcomes.
Software as Medical Device (SaMD) refers to software used for medical purposes without being part of a hardware medical device. This software can perform various functions, such as diagnosing conditions, providing treatment recommendations, and monitoring patient health. The SaMD market is experiencing rapid growth, with a projected compound annual growth rate (CAGR) that could see it reaching up to $6.1 billion by 2034.
The Internet of Medical Things (IoMT) encompasses a network of connected medical devices that collect, analyze, and transmit health data. These devices include wearable sensors, remote monitoring tools, smart implants, and other connected medical equipment. IoMT enables real-time health monitoring, early detection of medical issues, and continuous patient care.
An example of SaMD/IoMT in action is the healthcare organization that invested $270,000 in a scanner designed to detect changes in subepidermal moisture, an early indicator of pressure ulcers (bedsores).
This technology led to a 27% reduction in the prevalence of pressure ulcers, resulting in shorter hospital stays and estimated annual cost savings of $3.25-4.3 million. That’s an ROI of up to nearly 1,500%.
Benefits of SaMD and IoMT
Enhanced patient monitoring: IoMT devices enable continuous monitoring of patients’ vital signs and other health metrics, providing real-time data to healthcare providers. This allows for timely interventions and more proactive management of chronic conditions.
Early detection and prevention: SaMD solutions can analyze data from IoMT devices to detect early signs of medical conditions, enabling preventive measures and reducing the risk of complications.
Improved clinical decision-making: SaMD applications can process vast amounts of health data and provide actionable insights to clinicians. These tools support more informed decision-making, leading to better diagnosis, treatment plans, and patient outcomes.
6. Personalized Medicine
Personalized medicine, also known as precision medicine, involves tailoring medical treatment to the individual characteristics of each patient. It takes into account genetic, environmental, and lifestyle factors that can influence health and disease. This approach allows for more accurate diagnoses, more effective treatments, and better patient outcomes.
Key Benefits:
Targeted Treatments: Personalized medicine enables healthcare providers to select treatments that are most likely to be effective based on a patient’s genetic makeup. This reduces the trial-and-error approach often associated with traditional treatments.
Early Disease Detection: Genetic testing can identify predispositions to certain diseases, allowing for earlier interventions and preventive measures.
Reduced Adverse Effects: By understanding how a patient’s genetics affect their response to drugs, personalized medicine can help avoid adverse drug reactions.
A notable example is the use of personalized medicine in cancer treatment. The National Cancer Institute's MATCH (Molecular Analysis for Therapy Choice) trial matched patients with specific genetic mutations to targeted therapies, the results of which indicated that people with advanced cancer may benefit from genomic sequencing to help plan their treatment.
7. Healthcare Apps
Healthcare apps are mobile applications designed to help individuals manage their health and wellness. These apps provide a wide range of functions, from tracking physical activity and diet to managing chronic diseases and facilitating telemedicine consultations.
Key Benefits:
Enhanced Patient Engagement: Healthcare apps empower patients to take an active role in managing their health by providing them with tools to monitor and track their health data.
Improved Access to Care: Telemedicine apps enable patients to consult with healthcare providers remotely, increasing access to care, especially for those in remote or underserved areas.
Chronic Disease Management: Apps designed for chronic disease management help patients adhere to treatment plans, monitor symptoms, and communicate with their healthcare providers.
One example is the MySugr app, designed for diabetes management, which helps users track their blood sugar levels, log meals and physical activity, and share data with their healthcare team.
8. Cloud-based CRM Software in Healthcare
Cloud-based Customer Relationship Management (CRM) software allows healthcare providers to communicate with patients through personalized messages, appointment reminders, and follow-up notifications. Cloud-based CRM aids healthcare organizations in managing patient relationships more effectively, streamlining administrative tasks, and providing more personalized care.
These systems often include patient portals where individuals can access their medical records, schedule appointments, and communicate with their healthcare providers.
This technology helps us to truly focus on empathy and put the patient at the center of everything we do.
– David Hook, Executive Director of Marketing & Digital Consumer Experience at John Muir Health told Salesforce.
Benefits of Cloud-based CRM Software
Increase Patient Engagement: The CRM system enabled personalized communication with patients, leading to higher engagement rates and improved patient satisfaction.
Enhance Care Coordination: Integration with existing EHR systems provided a unified view of patient data, which improved coordination among healthcare providers and led to better patient outcomes.
Boost Operational Efficiency: Automation of administrative tasks such as appointment scheduling and follow-up reminders reduces the burden on healthcare staff and minimizes errors. 80% of healthcare organizations with cloud-based CRM software report that it has increased revenue and decreased costs by allowing staff hybrid access both on-premises and remotely.
The Importance of Digital Trends for Healthcare Organizations
Staying abreast of digital healthcare trends is crucial for healthcare leaders aiming to remain competitive and provide the highest quality of care. As we move forward, it is imperative for healthcare organizations to continue exploring and embracing new digital tools and strategies. By doing so, they can ensure that they are not only keeping pace with the digital evolution but also setting new standards in healthcare excellence.
The above examples of digital transformation in healthcare demonstrate its profound impact. From AI-powered diagnostic tools to remote patient monitoring systems, the adoption of these technologies is leading to improved patient outcomes, reduced costs, and streamlined workflows.
However, digital transformation is not just about technology. Its success hinges on how systems rolled out, the cultural attitudes toward digital innovations, and clear communication about what success looks like. Digital transformation starts from the top—the onus is on leadership to make solutions stick through transparency and accountability. Learn more about how to implement digital transformation in healthcare by downloading Product School’s free white paper, Uniting People and Technology for Transformative Change in Healthcare.
Updated: September 19, 2024




